The Future of Analytics
Virtual healthcare, also referred to as telehealth, is not merely a low-cost digital substitute for traditional in-person care. In fact, when utilized appropriately, it can drastically enhance patients’ overall health and experience, while also lowering healthcare costs.
The pandemic led to a significant proliferation of virtual healthcare worldwide. Telehealth services grew to reach 32.5 million by Feb ’21 within Medicaid and Medicare (15x pre-pandemic levels)(1). Today, 50M in-person visits/year could be converted to virtual visits(2). Furthermore, 40% of hospitals are expected to shift 20% of their beds to the patient’s homes by 2025(3).
Patients have also become more accepting of telehealth as a means of accessing healthcare services (particularly in remote or underserved areas), as it offers convenience and safety, and reduces the risk of exposure to any virus. What started as a pandemic trend is now here to stay. 60% of patients find virtual care more convenient than in-person care(4).
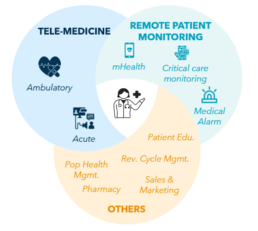
Today, telehealth refers to a broad term including a wide range of virtual health services including clinical services like medical consultations (ranging from high acuity care to low acuity i.e., ambulatory care) and non-clinical services like remote patient monitoring, and patient education. Telemedicine, on the other hand, is a subset of telehealth specifically referring to the use of telecommunications technologies to provide clinical healthcare services
such as medical diagnosis, treatment, and prescription by a healthcare provider.
Remote Patient Monitoring (RPM) allows healthcare providers to remotely monitor and track patients’ health status using wearables, smart devices, sensors, and vitals monitoring machines (for critical care). This data is transmitted to healthcare providers, who can then use it to make informed decisions about patients’ recovery.
In order to make the user experience more holistic, various ancillary services like insurance, billing, and pharmacy, are now embedded with telemedicine offerings to create a seamless patient journey. The industry is now moving towards a 365/24/7 care model, where-
Exhibit 1. Telehealth Capabilities
-telehealth capabilities pervade from the time a patient is getting hospitalized, to when he/she is back home needing to connect with a provider on demand even after recovering. Exhibit 2 shows how telehealth enables each stage of a patient’s care journey.
Exhibit 2. The Patient Care Journey
The Promise of a Brighter Future
Innovations in telehealth platforms are seeking to transform clinical care by shifting away from conventional care settings, clinical service providers, and business models. Innovative capabilities that will become mainstream in upcoming years include:
Exhibit 3. Priority Matrix for Digital Care Delivery(6)
A. Care Delivery
- Autonomous Monitoring: Surveillance of patient and provider behaviour using video and sensor technology to analyse and act on real-time intelligence derived from human activity and surroundings. Patient privacy, security and policy issues (related to real-time video surveillance), technical limitations of image recognition and sensor technologies, indexing and compliant storage of surveillance data are some of the obstacles that need to be tackled. Currently, the development of these monitoring systems for neonatal intensive care units that can detect signs of distress in premature infants is in progress.
- Care team collaboration: An interoperable application ecosystem (IAE) representing the convergence of conventional and evolving point-of-care, patient access, and middleware technologies. E.g., nurse call, interactive patient care, alarms and notifications, clinical communication and collaboration, and next-gen contact centers. Legacy application integration challenges, particularly the lack of open APIs, automation features, and understanding of the conceptual framework are hindering growth.
- Robotics-Assisted Telesurgery: It remains a nascent application; adoption will accelerate as current technical challenges are addressed. In particular, the ubiquitous adoption of 5G with its low latency, high reliability, and high bandwidth will address specific issues relating to latency.
- Successful pilots are currently driving excitement about robotics-assisted surgery. E.g., Apex Heart Institute in India successfully performed remote robotics-assisted coronary intervention with a surgeon located 20 miles away.B. Clinical Decision Support
- Automated Patient Decision Aids: help patients make informed decisions about their care by providing personalized treatment options, risks and benefits. The University of Washington’s Decision Aid Lab has developed several decision aids for patients with chronic conditions such as diabetes and osteoarthritis, which have been shown to improve patient knowledge and decision-making confidence.
- Precision & Genomics Medicine: Precision medicine is improving health outcomes by leveraging individual and patient factors to diagnose and treat medical conditions. One of its key components is genomics medicine, which includes gene sequencing, high performance computing, AI-informed risk assessment, and clinical decision support. As additional correlations between genetic biomarkers, disease prevention, and treatments are uncovered, the adoption of genomics medicine is expected to grow. However, challenges remain, such as technology adoption, cost and reimbursement of genomic sequencing, EHR integration, and managing the volume of data required
- Digital Telepathology: enables remote viewing, manipulation, interpretation, and automated image analysis of digitized laboratory specimens. Primary diagnosis using digital telepathology is now allowed in the U.S., EU, and Canada. With advancements in cloud technologies and edge computing, digital telepathology programs are expected to grow since large, high-resolution digital images need to be transmitted.C. Digital Infrastructure
- Digital Health Platform: Architectural approach that enables healthcare providers to rapidly respond to strategic imperatives and external uncertainties using modern cloud platforms and services. DHPs will rise swiftly up and over the peak by leading vendors such as Amazon, Google, Microsoft, Philips, and Salesforce as drivers combine with the availability of regionally compliant, highly secure, and available cloud SaaS and PaaS solutions.
- Smart electronic health record (EHR) user interface (UI): solutions use AI/ML to synthesize, summarize and elevate relevant clinical data from the EHR and other clinical data sources, creating a contextualized view of the patient record. With the increasing physician burnout, such solutions become critical where physicians are spending, on average, 1.8 hours per day outside of office hours completing documentation.
- Digital Clinical Voice Analysis: uses AI and ML to analyse voice patterns and identify voice biomarkers that can non-invasively detect clinical abnormalities for diagnosis. It can predict disease onset, measure symptom severity, and monitor treatment response. This technology is affordable, portable, and scalable, making it ideal for virtual care. Advances in smartphone and home voice assistant technologies have made accurate recording and real-time interpretation of vocal data more accessible. The CoLive Voice study is collecting and analysing voice recordings of 50,000 individuals globally to advance the use of voice for diagnosis, risk prediction, and remote monitoring of multiple conditions.
- Semantic Interoperability: Ability of different information systems to exchange and process business and clinical information with a common understanding. Well-defined and enforceable standards and terminologies are increasingly essential across care ecosystems and system vendors. Factors driving the adoption include the increased focus on population health, investment in health information exchanges, and the growing demand from consumers for patient-held records including the ability to store copies of their medical records on consumer-managed devices like the Apple HealthKit.
Everyone Should Benefit...
The benefits of virtual healthcare are well-known:
- Improved Access to Healthcare: Telehealth provides patients with healthcare services regardless of location. This is especially beneficial for patients who live in rural or remote areas or who have difficulty traveling to a healthcare facility. HCA Healthcare saved 2-5 hours of travel time from rural locations via its telehealth program to improve the clinical efficiency of obstetrics patients who live far from care facilities.(7)
- Cost Efficiency: Beneficial for both patients and healthcare providers as it eliminates the need for travel and reduces administrative costs including admissions, re-admissions, transfers, and emergency department visits. Spectrum Health saw ~$1M in cost savings using an ED discharge program.(8) Continued telemedicine usage will reduce healthcare spending anywhere from 15% – 20%.(9)
- Improved Patient Engagement and Satisfaction: Telehealth enables hospitals to deliver a more timely, efficient, convenient, personalized, and accessible care experience. For example, Pediatric Associates decreased wait time by 75%, and reduced ER use by 60% among high ER utilizers for low-acuity conditions using telehealth. (8)
- Improved Care Coordination & Health Outcomes: Telehealth can help improve care coordination among healthcare providers, which can lead to better health outcomes for patients.
For example, Palo Pinto General Hospital’s telemedicine partnership resulted in a reduction of emergency department patient transfers by 36% annually.(10)
...However, Not Everyone Does
A few roadblocks continue to impede the widespread adoption of telehealth:
- Inertia: To date, telehealth is frequently viewed and used as a digital channel for disbursing traditional health care. Additionally, the adoption of telehealth channels is often left to the individual provider. Now that the concept and technology for telehealth are well-proven, hospitals should transition to a telehealth-first model that seamlessly integrates the end-to-end care journey.
- Technical: Better data integration and improved data flows are needed across the ecosystem to provide the needed experience. Common issues faced today include:
- Lack of endpoint configuration with software
- Lack of customization and inability to integrate with in-house technologies (e.g., patient portal)
- Lack of EHR integration with software
- Lack of web-based platform (App needs to be downloaded)
- Lack of dynamic bandwidth capability
- Non-cloud-based platform
- Training and Operational: Clinicians and hospital staff need to be prepared before and after implementation. Some platforms require provider and administrative training to handle their complex interface. Additionally, some platforms can suffer from excessive downtime.
- Data and Security: Infrequent or insufficient security patching and offshoring of EHR, can lead to cyber vulnerabilities.
The Industry is in Motion
As with most industries, the early gold-rush generated a plethora of small and medium-sized providers offering a range of capabilities. Now as the industry is maturing, it is undergoing rapid transformation. Legacy health-tech providers are gobbling up young upstarts, large desktop videoconferencing firms are starting to build vertical use cases in healthcare, and specialist telehealth platforms are rapidly expanding their capabilities via partnerships, acquisitions, and in-house development.
In particular, there has been a significant consolidation, with heavyweights:
- Big tech: Microsoft acquired Nuance for $19.7B for its conversational AI and cloud-based clinical intelligence. This enables Microsoft to pursue the growing demand for patient engagement solutions to help hospitals with their digital front door. Google debuted an AI-powered dermatology assistant that allows users to upload images of the skin, hair, or nails and answers a series of questions and for each matching condition, the tool will show dermatologist-reviewed answers. Apple’s focus is utilizing iOS’ HealthKit, ResearchKit, CareKit, and the Apple Watch to collect data beyond just heart rate and oxygen levels to assess user health trends and risks. Verizon’s BlueJeans Telehealth subsidiary has announced a new integration with Apple Health that lets patients share their health data with healthcare providers during a telehealth consultation with the company.
- Desktop Video Conferencing: Video conferencing tech giants Microsoft Teams and Zoom have expanded their offering to become a virtual telehealth platform for e-consultation. CrowdOptic developed a video integration solution to livestream surgical procedures over Zoom for clinical support and physician training. Microsoft Teams has also partnered with Teladoc to provide ‘Solo’, an EHR-integrated telehealth platform.
- Data Management: Oracle Cerner, a leading EHR provider has now expanded its offering to acute and ambulatory care telehealth services through its cloud-based platform called HealtheLife. The platform is designed to access a range of health services remotely, including virtual consultations, telemonitoring, and e-visits. In addition, Oracle Cerner also offers other telehealth solutions, including tele-pharmacy, tele-stroke, and tele-behavioral health services.
- Others: Philips has one of their offerings called the eICU which allows intensivists and critical care nurses to monitor patients in the ICU remotely, using advanced analytics and patient data to identify trends and provide timely interventions. The program also enables real-time collaboration between remote intensivists and on-site ICU staff, helping to improve patient outcomes and reduce costs. In addition to the eICU program, Philips also offers other telehealth solutions for remote patient monitoring, virtual consultations, and telehealth education.
Exhibit 4. B2B Telehealth landscape
Health Systems are Actively Modernizing
- Northwell Health has been taking several steps to advance the quality of healthcare and improve patient outcomes. The health system deployed Teladoc Health’s virtual care platform to expand its telehealth offerings and improve communication between clinicians. This allowed Northwell to leverage integration with Microsoft for “hyper-personalized” care. Furthermore, a partnership with Royal Philips resulted in a 20% reduction in ICU mortality rate. Additionally, Northwell Health piloted a wearable biosensor program within emergency departments, resulting in a 73% improvement in patients’ feeling of being well taken care of. The research department has developed an AI tool to gauge when patients need to be woken up during the night, reducing the workload of clinicians by 20-25% per overnight shift.(11)
- Trinity Health partnered with Vivify Health to provide home care patients a mHealth platform offering a real-time link to a nurse; featuring a pre-programmed wireless 4G-enabled tablet and other wireless devices for collecting patient data.
- Mayo Clinic has implemented a variety of actions to improve healthcare and patient outcomes. One of the significant changes is consolidating its telemedicine vendors into one provider, InTouch Health, a subsidiary of Teladoc. This move allows them to provide consistent, high-quality telemedicine support across nine states. Additionally, their partnership with MediView, a clinical augmented reality med-tech company, enhances remote collaboration and visualization. This collaboration aims to improve holographic interventions and provide patients with innovative treatment options. They are collaborating with NXgenPort, a BioMedTech firm, to support the development of a cancer-focused remote patient monitoring tool with an implantable chemo-port catheter. Additionally, they have a 10-year agreement with Mercy to power personalized, predictive medicine by using data analytics.
- Advent Health has entered a partnership with Advanced ICU Care, (Hicuity Health), to provide high-acuity telemedicine services for ICU patients. This collaboration uses remote monitoring technology to support bedside providers and nurses and the collaboration with Monogram offers care coordination, telehealth, and remote monitoring for patients with chronic kidney and end-stage renal disease.
Do You Have the Right Telehealth Platform?
The right telehealth platform is critical to meeting patient expectations and providing the best possible provider, patient and administrator experience. Today patients are demanding more control over their healthcare and want to access care from anywhere.
Exhibit 5. How to confirm if you have the right telehealth platform?
In Closing...
Telehealth is a critical and pervasive component to future-proofing healthcare delivery. Today, most hospitals underutilize this capability. Given the rapid evolution of telehealth capabilities and the players providing them, most hospitals are realizing that their current platform may not be well integrated, limited in capabilities, and with a clunky user experience that is limiting adoption and user satisfaction.
Given the significant shift in the industry, we recommend proactively revisiting/confirming your choice of telehealth platforms. The capabilities currently available in the market, and those under development, promise to significantly enhance patient care, increase access to healthcare services, and lower costs.
With the plethora of options available, it can be difficult to determine the right platform(s) for your needs. A careful evaluation of platform capabilities, available integration, hardware independence, data security, service, and support is needed to make an informed decision.
With the right platform, healthcare providers can accelerate the adoption of virtual healthcare, and redesign their care model to be patient-centric and efficient.
__________________________________________________________________________________________________________
- GAO (US Government Accountability Office)
- American Psychiatric Association
- Gartner 2022
- McKinsey Survey 2022
- Device used for e-consultation for inpatients – wall mounted/cart-attached monitors, bedside tablets etc
- Gartner Hype Cycle for Digital Care Delivery
- Teladoc website
- Amwell website
- HealthCare IT News
- Access Telecare website
- ML algorithm uses a modified early warning score (MEWS) along with the previous night’s vital sign data and information on heart rate and elevated blood pressure to inform a clinician’s decision on whether to disturb a patient’s sleep